
Healthcare mobile app development
- Home
- Healthcare software development solutions & services
- Healthcare mobile app development
With 25+ years of experience in healthcare app development services, Itransition delivers tailored mobile healthcare (mHealth) solutions that help providers expand their services and improve care accessibility through mobile applications integrated with existing healthcare systems and wearables.
Table of contents
Itransition as a healthcare mobile application development provider
25+ years of experience in software development
Forrester's Modern Application Development Services report recognition
FDA- and HIPAA-compliant software
Adherence to OWASP and other app development security guidelines and frameworks
Working knowledge of DICOM, ICD-10, CPT and other major healthcare standards and coding systems
Clinics
Pharmacies
Labs
Private practitioners
Research organizations
Patients & their caretakers
Wellness centers
Rehabilitation facilities
We develop mHealth apps for
Mobile healthcare applications we develop
We deliver mHealth applications for iOS and Android, either stand-alone or complimentary to larger software suites, ensuring their compliance with HIPAA, GDPR, CCPA, and other applicable data security and privacy regulations.
For patients
Itransition’s medical app developers deliver mobile solutions that allow patients to access their medical records, communicate with medical professionals and health insurance providers, and track their treatment plans. Additionally, our development team integrates healthcare mobile apps with wearables and healthcare IoT devices for personalized, streamlined healthcare delivery.
- Appointment scheduling and management
- Access to the EHR data
- Medication intake reminders
- Prescription orders
- Educational materials
- Secure messages between patients and doctors
- Remote patient monitoring
For medical staff
Itransition develops healthcare mobile applications that enable healthcare professionals to provide care and support to patients anywhere, while automating routine tasks to give physicians and nurses more time for meaningful patient interactions.
- Real-time patient data monitoring
- Secure access to electronic health records and PHI from outside the office
- Remote collaboration and secure health information exchange
- Virtual consultations
- E-prescribing
- Meeting and appointment booking
For healthcare organizations
Our mobile digital solutions help automate clinical and administrative workflows, provide actionable insights for efficient facility and practice management, and enhance operational efficiency across hospitals and clinics.
- Laboratory operations management
- Medication stock assessment
- Inventory order placement
- Equipment and other assets tracking
- Team management and task tracking
Need a mobile app to enhance your health care delivery?
Our mHealth software development success stories
Itransition develops tailored healthcare solutions that address complex clinical and administrative challenges, helping our clients deliver better care and operate more efficiently.
3x
faster case creation
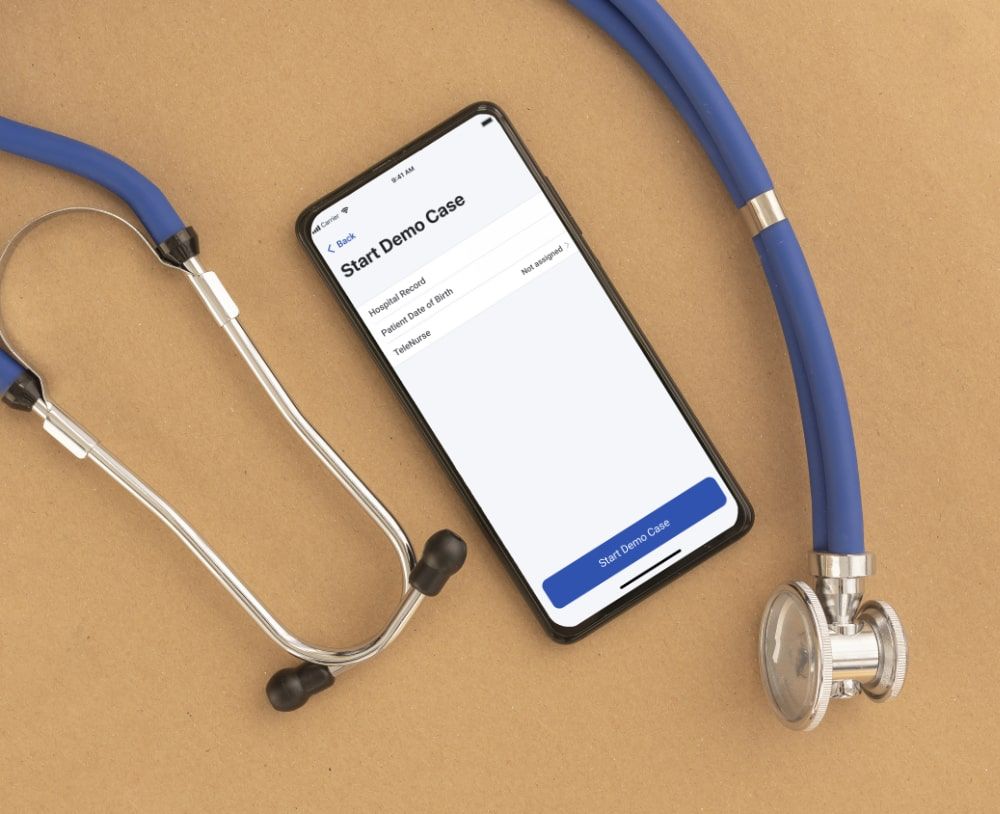
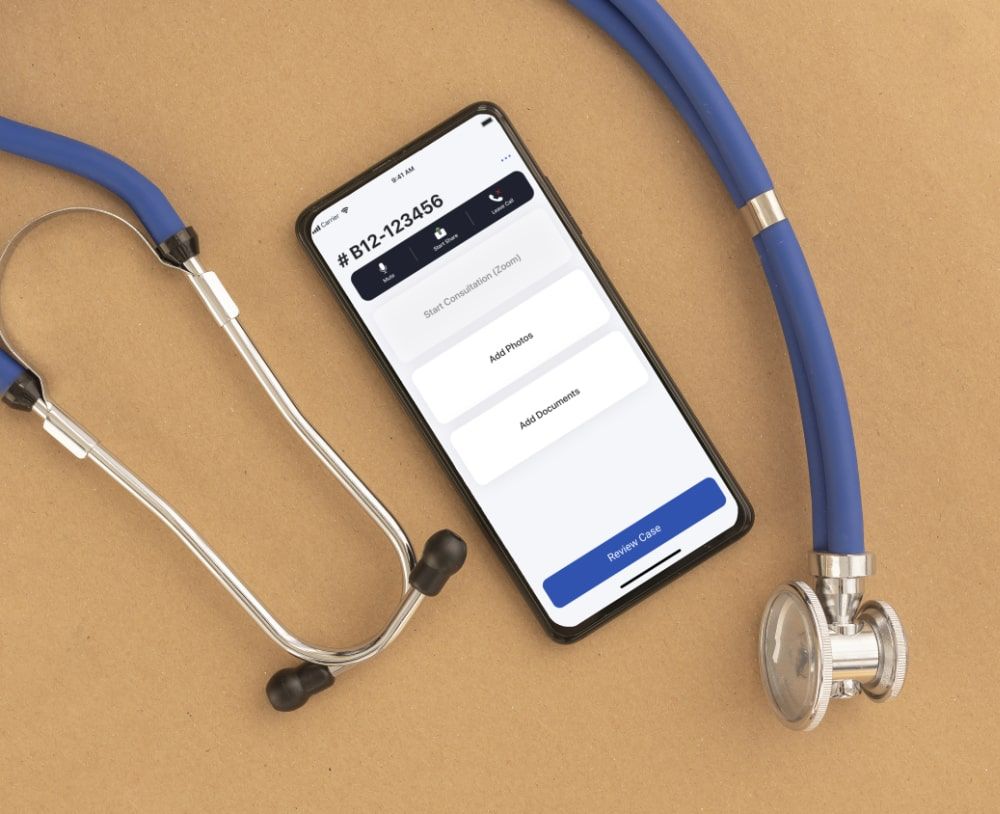
Telehealth suite for remote patient monitoring
We developed a mobile teleconference solution for nurses in rural areas to provide care to assault victims and properly collect evidence through remote assistance via the app, ensuring its HIPAA compliance.


2x
more reports submitted
Adverse event reporting app
Our team delivered a cross-platform mobile app that complements the client’s web-based healthcare system for adverse event reporting and provides patients and healthcare professionals with real-time access to adverse event data.
Essential integrations for mHealth software solutions
The flawless integration of the mHealth apps with other medical software improves the interoperability within the healthcare organization, enhances the effectiveness of the digital health solutions, and contributes to informed decision-making, better patient outcomes, and increased healthcare providers’ productivity.

We help providers enhance their interaction with patients with the help of high-quality video and audio conferencing capabilities realized in the iPhone or Android apps, allowing doctors and nurses to be even more flexible in their work locations and schedules.
Our experts create app designs compatible with the popular remote patient monitoring equipment (ECG and heart rate monitors, glucose meters, fitness trackers, etc.) that collect and store patient health data for further processing by healthcare professionals.
Itransition’s healthcare app developers enable patients to access all functionality of the patient portals, including scheduling appointments, rating visits, and accessing test results or educational information, from their mHealth app.
Our experts connect mobile apps to analytical algorithms that process healthcare data, enabling clinicians to make data-based conclusions and predictions, improving medical care, and visualize the results via user-friendly mobile interfaces.
The CRM-mHealth app integration enables healthcare professionals to easily access patient information and deliver high-quality customer care on the go.
Our team can deliver medical mobile apps compatible with your EHR/EMR software for patients and medical personnel to manage patient health records in line with HIPAA regulations, schedule appointments, and view treatment prescriptions anytime from anywhere.
Looking for experienced healthcare mobile app developers?
Advanced technologies for healthcare applications
Our expertise in medical product development, coupled with our knowledge of the latest technological advancements, enables us to deliver customized solutions that address complex business problems and help our clients stand out from their competitors.
We build apps synced with sensors and wearable devices, including AI-powered activity trackers in sports, for real-time health monitoring, timely diagnostics, and disease monitoring. Combined with big data management and analytics, this technology provides visibility into population health and assists with medical facility management.
We use AR, VR, and 3D imaging technologies to support the management of mental health conditions such as anxiety disorders, enhance rehabilitation outcomes, and provide immersive, interactive training and educational experiences for both staff and patients.
We apply AI technologies, including machine learning and NLP, to augment mobile apps with healthcare AI-powered chatbots and virtual assistants that can answer frequent questions or help patients accomplish simple tasks within the app, increasing patient satisfaction while decreasing medical staff’s overloading.
Our custom mHealth app development process
Itransition’s mobile health app developers can provide an end-to-end implementation of mHealth solutions spanning business analysis, on-demand MVP creation, full-scale application development, and post-deployment assistance and maintenance.
1
Research & analysis
We conduct a business needs analysis to define requirements for the healthcare application, conceptualize the app idea, design the solution, including the UX design, and determine the optimal technology stack. At this stage, we also specify software security requirements, including authentication and role-based access control, to ensure the application’s safety and compliance.
2
Project planning
Our experts outline the development project’s scope, deliverables, and timelines and assemble a project team to carry out the implementation. If required, we also create a PoC at this stage to validate the solution’s feasibility and reduce project risks.
3
Application development
During the solution’s backend and frontend development, we implement all of the solution’s required functionality and ensure the app’s scalability and compatibility with the rest of the organization’s IT ecosystem.
4
Testing
We accompany our mobile healthcare application development process with continuous quality assurance to ensure the apps’s security, regulatory compliance, reliability under heavy traffic loads, and usability of all app components.
5
Launch
We integrate the finished application with the healthcare organization’s systems and release it to end users. If needed, our experts migrate data from legacy software, ensuring its accuracy, and conduct acceptance testing to confirm the solution’s quality.
6
Post-implementation support
After the successful app implementation, Itransition can provide varying levels of support including a 24/7 dedicated service team to address any challenges that may arise, perform iterative upgrades and integrations with other software if needed, performance monitoring, and other services according to the stakeholders' needs.
Mobile healthcare software development benefits
We help healthcare companies improve patient care and gain numerous advantages to get ahead of their competitors.
Process & cost optimization
Digital transformation, and mHealth solutions in particular, allow medical specialists to provide care from anywhere, which optimizes their workday and frees them from routine tasks. Our mobile apps also enable staff to take preventive measures to intercept the regression of patients’ health conditions and avoid unnecessary hospitalizations, streamline everyday operations, and use equipment and resources more efficiently.
Improved health outcomes
Itransition implements mHealth software that encourages patients to become more proactive in managing their own health which leads to healthy lifestyles and improved population well-being. Automated notifications about medication intake, immunizations, or appointments also enable more continuous and correct treatment resulting in fewer readmissions to the hospital, urgent cases, and adverse reactions.
Enhanced patient engagement & loyalty
By developing mHealth apps, we help providers facilitate convenient and clear communication between healthcare organizations and their target audience, which improves patients’ trust, loyalty, and willingness to participate in treatment and research procedures.
New business opportunities
We create mobile apps to enhance your existing services, find new ways of monetization, or expand your service offer with mobile care. Advancements in your digital health offering can also attract new patients or convince loyal clients to sign up for more advanced care options.
Related services

Hospital management software
Itransition delivers hospital management software for medical departments to collaborate, coordinate, and automate inventory and contract management, securely share data, and optimize resources’ usage.
Pharmacy management software
We deliver document, inventory, and financial management solutions for pharmaceutical organizations to streamline inventory management and order placements, keep track of controlled substances, and automate routine processes in customer requests’ fulfillment.
Medical image analysis
Our experts develop intelligent image analysis solutions that facilitate more accurate diagnosis, streamline patient testing, and lower image processing costs for medical organizations.

Medical device software development
We enable healthcare organizations to enhance the monitoring of health metrics, patient treatment, and disease diagnostics using medical devices supported by safe and resource-efficient custom software.
Offer convenient health care via custom mHealth applications
FAQs
As a healthcare mobile app development company with years of experience, we can clarify many questions to our clients at the beginning and during our partnership. Here we shortly answer the most popular ones.
How much does it cost to develop an mHealth app?
The estimated development cost of a mobile medical app can vary significantly depending on its functionality, the type of information the application handles, the tech stack needed to cover all of the key features, the variety of platforms it has to operate on, the number of existing systems it has to be integrated with via APIs or custom connectors, and user experience (UX) design requirements to ensure the app is intuitive and accessible for all user groups. If you need to get a ballpark price for your project, contact Itransition’s consultants.
Why hire medical app developers instead of using a ready-made solution?
A ready-made solution cannot cover your organization’s and users' needs perfectly. Opting for custom healthcare app development, you ensure that the application meets your company’s unique requirements and regulations of a particular region, integrates flawlessly with your other healthcare equipment and software, and is fully personalized, enhancing user experience and satisfaction.
Do you provide healthcare mobile app development services for enterprises only?
Itransition is a mobile app development services company that provides services to enterprises, SMBs, and startups based on their specific needs. Reach out to us to learn how we can become partners.
What are the most common types of mobile health applications?
There are medical applications in app stores for almost any area of healthcare industry, including:
- Mental health management solutions
- Wellness apps
- Fitness apps
- Remote condition monitoring apps
- Telemedicine apps
- Sleep tracking apps
- Menstrual cycle tracking solutions
- Software to access EHR and other medical data
- Informational and educational apps
- Task and team management apps
- Hospital inventory monitoring mobile solutions
- Healthcare ecommerce apps

Case study
Sharing economy workout app development
Find out how Itransition developed an MVP of a sharing economy workout fitness app that brings together trainees and fitness trainers.

Case study
Asthma monitoring software suite
Discover the tips and tricks behind asthma monitoring software developed by Itransition’s team to help asthma patients self-manage their condition.

Case study
Wellness platform development for a US healthtech company
Read how Itransition developed a SaaS wellness platform for a US healtech startup, now boasting 100,000+ registered users.
More about healthcare software services
Services
- Healthcare software development
- Healthcare mobile app development
- Patient portals
- Hospital management software
- Hospital inventory management software
- CRM
- Data analytics
- Remote patient monitoring
- Medical image analysis
- Pharmacy management software
- Medical device software development
- Patient engagement solutions
EHR
Telehealth