The ever-growing cost of health care has always been a major pain point for the industry and the US economy, and in recent years, it has only gotten worse. When Statista studied the correlation between the cost of healthcare and the gross domestic product (GDP) over the last sixty years, they discovered that the share of healthcare cost in the US GDP was steadily growing, having stabilized at around 17% from 2009-2017. In 2020, however, the share increased by 2% and reached $4.1 trillion in monetary terms:
The sum is immense, especially amidst the pandemic, but this is not the worst part. As a JAMA publication from October 2019 reports, a quarter of this investment is wasted annually. According to the authors, there are six domains of healthcare waste, namely the failure of care delivery and coordination, overtreatment or low-value care, pricing failure, fraud and abuse, as well as administrative complexity.
Is it possible to reduce this waste? In today’s highly digital age, healthcare software development and digital transformation appear to be the most fitting solution to this long-standing issue. Let’s see how digitization is improving healthcare cost-efficiency and whether this effort pays off.
Digital transformation in healthcare: where are we now?
Digital transformation in healthcare is a complex process that requires extensive efforts and investments. Nevertheless, health system CEOs are quite positive about the transformation. According to Scottsdale - Deloitte’s 2021 Healthcare Systems Survey, about 50% of the participants believe they will complete the transformation in three to five years:
This is how industry leaders put it:
A monumental shift is occurring across the industry as more and more organizations adopt digital health strategies that transform health and care.
Patient experience digitization
Today, as the world has seen the limits of curative medicine, disease prevention is viewed as a means to reduce healthcare cost and is therefore gaining momentum.
However, healthcare professionals should not be the only ones driving this effort forward. Active participation from patients is also crucial for the success of healthcare’s digital transformation. To this end, patient engagement solutions should be an important addition to a hospital’s software toolkit.
Patient portals and mobile apps became essential for patient engagement in the years 2020 and 2021. However, the road to success was full of roadblocks and pitfalls due to the lack of coordination between the key actors – healthcare providers and patients.
With the pandemic spreading across the country, patient-centered solutions were the only sources of trustworthy information about the virus in the vicinity. Besides, they allowed patients to address their health issues with minimal virus exposure via telemedicine consultations and/or health wearables.
Though the pandemic is now under control, patient engagement solutions haven’t lost their relevance. Patients have learned to manage their health independently and proactively, taking responsibility for their own health and viewing doctors as assistants, not the key decision-makers.
Mobile healthcare apps
With 97% of the population owning a cellphone of some kind, mobile apps are the perfect devices to bridge gaps in health care access. However, while hospitals have been engaging in healthcare mobile app development for over a decade, in the majority of cases, these solutions have typically failed to win patients’ trust. Hence, retention rates were low for both patient portals and healthcare apps.
In 2020-2021, providers have reconsidered their approach to patient-centric healthcare mobile apps and added a range of new functions that reflected patients’ needs. Interestingly, some capabilities were included for the first time:
As we can see, “the 2021 newcomers” are aimed at facilitating patient-provider interactions in one way or another, from finding your way around a clinic and location sharing to participating in health management campaigns. In addition , the subsequent mobile app adoption rate, according to CHIME, grew by 9% on average from 2020-2021.
Patient portals
In contrast, patient engagement portals have been in place for years. By 2018, patient portals made part of a digital mix for about 90% of surveyed providers, Medical Group Management Association (MGMA) Stat poll discovered. However, the tools’ popularity left much to be desired, only reaching the maximum engagement rate of 30%, the same source reports.
From 2020-2021, healthcare providers refocused and equipped their healthcare portals with new features. As for the updated solution’s popularity, СHIME Digital Health Most Wired Report paints a bright picture. According to CHIME researchers, in 2021, the use of portals in acute care and long-term and post-acute care (LTPAC) hospitals increased by 25%, reaching 83% and 82% accordingly:
Tips for enhancing patient engagement tools
According to the 2019 Digital Health Consumer Survey by Accenture, these are the top four functions patients want in their healthcare solution:
- Secure communication with the provider
- The ability to schedule and cancel appointments
- Electronic prescriptions
- Access to health records
Based on these findings, we have provided some practice-based tips to keep in mind. We have also added patient education modules to the list because of the positive feedback from researchers and providers who implemented this feature.
You will notice that approaches to ensuring the success of patient portals and mobile apps are interestingly similar. The reason for this lies in their common goal of engaging as many patients as possible, which allows medical providers to employ similar approaches to provide great UX and appeal to the target audience of either tool.
- Secure doctor-patient messenger
In fact, the significance of such interactions is often underrated. In their 2020 Digital Health Consumer Survey, Accenture found out that 55% of patients are eager to use health IT solutions recommended by reputable clinicians. At the same time, only 11% of medical professionals give such recommendations.
What’s more, combining portal-based messages with non-real-time interactions (asynchronous care) causes positive changes in patients’ behavior. Research published on JAMA Network in February 2022 reported that combining in-portal doctor-patient messaging with asynchronous care via smoking cessation surveys is twice as effective as patient outreach programs alone.
- Appointment scheduling assistant
With such tools at hand, patients can set appointments with the necessary specialists 24/7 without leaving their home, which makes care more accessible.
Such a tool offers benefits for providers as well. After scheduling an appointment, patients may forget about it and skip the consultation. For providers, such no-shows mean the loss of 12-18% of daily revenue, an article published on PMC in June 2020 reports. But the reminders built into the tool can help providers reduce no-show rates, increase their revenue, and lower administrative waste.
- Patient education tools
Traditionally, patients with serious or chronic illnesses are more interested in education programs. However, at some point, any patient may require some health-related tips. For example, patient education can assist patients during pre and post-operative care . According to the article published on JAMA Network in June 2021, sending a series of nine educational messages to patients before their colonoscopy procedure considerably improved the preparations and the procedure quality.
- Easy access to the patient’s EHR and medical history
Having access to their medical records and medical history allows patients to track changes in their health and make informed decisions about treatments and procedures. Custom EHR software allows patients to take a better look at their condition and manage their health independently while being able to turn to a medical professional at any time.
- E-prescription with automatic refills
When it’s time to refill a prescription drug, the tool can notify the patient who then sets the delivery time and date. This tool helps patients save time by not having to travel to their health care provider’s office and waiting in line.
Service digitization
In the years 2020 and 2021, healthcare providers witnessed the full potential and power of IT solutions in the healthcare domain. As patients continue to show interest in virtual care, AI-powered bots, and medical devices, healthcare providers have extended their efforts in those directions.
The main technologies many providers have already adopted are AI chatbots, IoT, telemedicine, and data analytics.
AI-powered chatbots
These smart tools can facilitate smooth communication with potential patients, guiding them across a healthcare facility, symptom-checking, and triaging. Thanks to natural language processing capabilities, RPA in healthcare via bots can provide 24/7 support and swift answers to most of the patients’ questions. By cross-linking a patient’s answers to their questions, bots can determine the appropriate order of treatment.
For example, Scout, an AI-powered digital assistant from Intermountain Healthcare in Utah was trained to evaluate the symptoms a patient reported. Based on the received information, it would suggest getting some good rest, setting up a doctor appointment or, in cases of health emergency, making a trip to the ER or an urgent-care facility.
Another virtual assistant deployed in Weill Cornell Medicine, New York City, can direct a patient to a doctor even when the person doesn’t know the exact name of the professional they need. For instance, in case a patient requires an appointment with an “eye doctor”, the Assistant offers them a set of options:
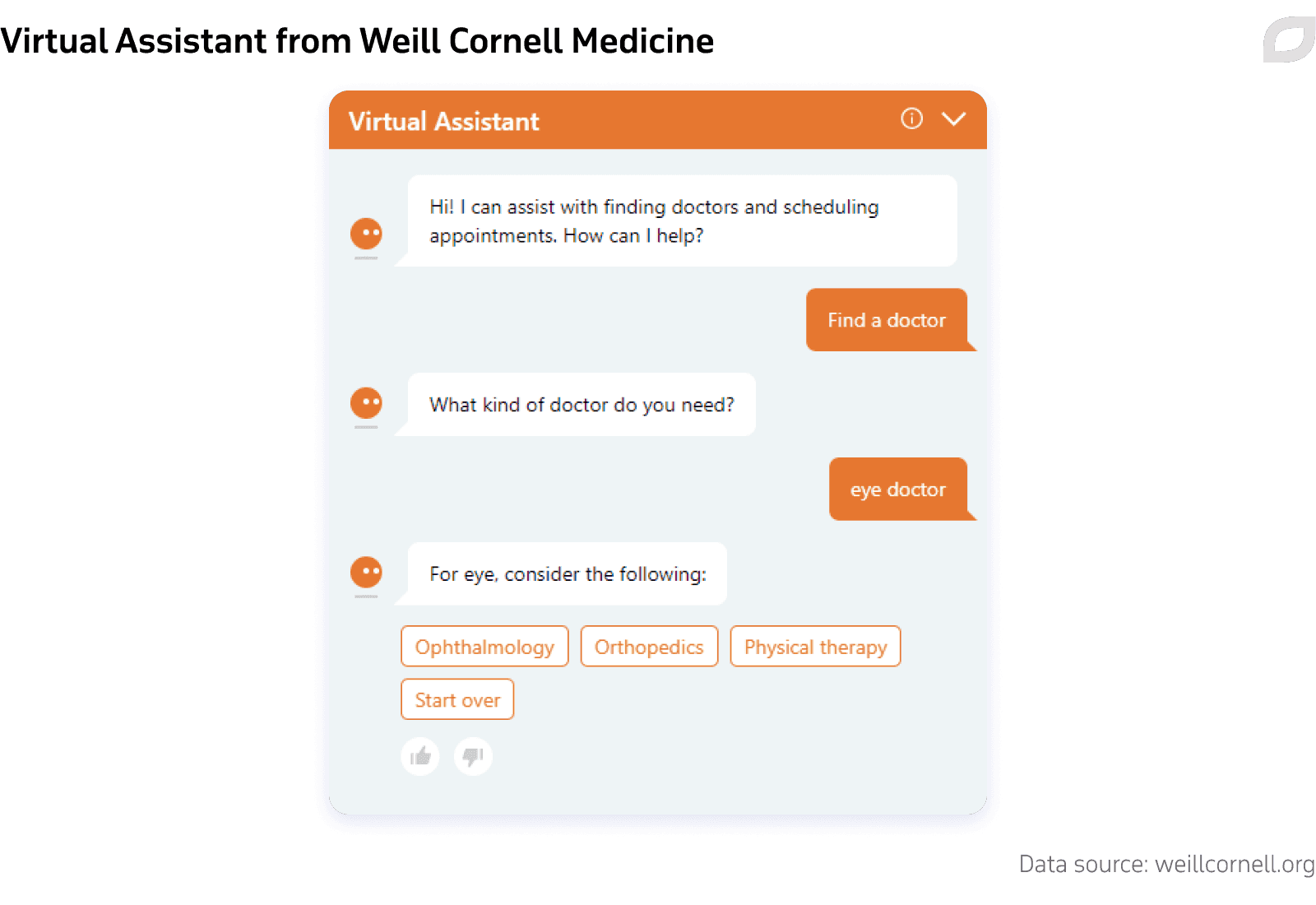
Deploying virtual assistants allows healthcare providers to lower labor costs and reduce one of the largest categories of waste: administrative complexity.
Telemedicine solutions
Telemedicine became the only viable tool for non-urgent care delivery during the peak of the pandemic in April 2020, reaching an over 30% influx in use.
Some experts believed the rate of virtual visits would drop once the public health emergency eased . Though some downscaling did happen, the use of telemedicine apps stabilized at a level exceeding the initial one by 38 times, McKinsey reports. As a result , the future of telemedicine looks much brighter than initially expected. However, the ways of delivering the service are still being established:
It's not whether telehealth will be offered, but how best to offer telehealth services as we move toward what we're terming digitally enabled care – […] fully integrated in-person and virtual care based on clinical appropriateness.
Though video solutions were developed for almost any field, including pediatric telemedicine, they don’t suit every patient. For instance, in remote or rural areas, patients often have difficulties connecting to the internet. Connectivity issues disrupt telemedicine provision, so patients from remote locations are left underserved.
To resolve the issue, providers have come up with offering audio-only consultations via a cellphone or a landline phone. Such doctor-patient interactions are recognized as viable solutions for managing behavioral and mental disorders, diabetes, substance abuse, and more. As the Centers for Medicare and Medicaid Services report, about one-third of such patients from locations with connectivity issues used audio-only consultations amidst the public health emergency. However, for areas of medicine where patient observation is critical (e.g. teleneurology), low connectivity still significantly limits care providers.
Medical IoT
The introduction of medical IoT has revolutionized the industry facilitating independent health management and timely care delivery. Those devices based on healthcare IoT have become essential for vulnerable patient groups such as patients with chronic conditions. The tools assist patients with monitoring critical health parameters and notifying their doctor or the emergency unit if needed. They can also fuel AI-based sports analytics solutions with biochemical data to track athletes’ conditions.
What’s more, software design for medical devices has witnessed certain democratization. It’s no longer necessary to buy a specific gadget to track one’s health parameters. A regular smartphone can do this job, as it contains a range of in-built sensors:
Typical present-day smartphone sensors
Regular smartphones with embedded sensors can work as monitoring devices for a range of conditions:
Smartphone sensors for health monitoring
| Monitored health issues | Typically used smartphone sensors |
|---|---|
| Cardiovascular activity, e.g. heart rate (HR) and HR variability (HRV) | Image sensor (camera), microphone |
| Eye health | Image sensor (camera) |
| Respiratory and lung health | Image sensor (camera), microphone |
| Skin health | Image sensor (camera) |
| Daily activity and fall | Motion sensors (accelerometer, gyroscope, proximity sensor), GPS |
| Sleep | Motion sensors (accelerometer, gyroscope) |
| Ear health | Microphone |
| Cognitive function and mental health | Motion sensors (accelerometer, gyroscope), camera, light sensor, GPS |
Medical data analytics
The pandemic has highlighted the role of healthcare data analytics for improving patient outcomes, population health, and overall facility performance. Analytical solutions can drive meaningful insights for decision-making on patient populations and individual patients. According to Markets and Markets’ report, global healthcare analytics is set to experience a 3.5-fold growth from 2021-2026:
During the pandemic, medical providers started to expand the number of sources they collected data from to take into account not only purely medical data, but also research papers, news articles, clinical trials, social media posts, and more. With today’s availability of medical data tools, experts can go for broad data collection to create full-scale patient profiles that reflect patients’ medical history as well as socioeconomic and environmental background.
These very factors, not considered by the healthcare system before, often predetermine patients’ behavior and health outcomes. For instance, analytics experts from Kaiser Foundation discovered that minority groups were the most vulnerable. In 2021, they had a larger share in cases, hospitalizations, and the mortality rate compared to white Americans:
Covid-19 cases, hospitalizations, and deaths by ethnicity, 2021
To improve the situation for such population groups, healthcare providers need to collect SDOH data on their patients. Some analytics tools can help with detecting pressing medical issues for local populations. Thanks to automated SDOH collection and healthcare big data analytics solutions, researchers from the National Institutes of Health detected a concerning tendency among Black and Hispanic teenagers in seven US states. According to a 2021 article published in JAMA, the number of cases of type 2 diabetes in those teenagers nearly doubled from 2001 to 2017. The researchers stated the reason for the upsurge was the extra weight those teenagers carried.
The researchers from Stanford Children’s Health also use SDOH data to create full-scale patient profiles and find out if a child needs any assistance other than medical (detecting cases of home violence, etc.)
Predictive analytics
Predictive analytics can assist clinicians in medical decision-making and patient outcomes improvement.
During the COVID-19 crisis, healthcare providers started identifying patients at high risk of getting infected by the virus and/or having poor health outcomes if they contracted it. Thus, researchers from Michigan Medicine deployed a specific PICTURE algorithm to predict patient deterioration accurately and prevent it if possible. The algorithm works for both COVID-19 and general wards.
In COVID-19 wards, the tool processes a whole set of data, from vital signs and lab results to demographic information. Relying on this data, PICTURE could detect patients at the highest risk of decline (intensive care unit transfer, respiratory failure, or death) and name the risk factors that define the prediction. This can help speed up the clinicians’ response and mitigate the waste of poor care delivery.
With the help of predictive models in healthcare, providers can detect not only the actual at-risk patients but also rising-risk patients. Identifying such patients in a timely fashion can help providers with reducing care costs and preventing unplanned hospitalizations, or the waste of overtreatment.
Using predictive analytics algorithms, researchers from Brigham and Women’s Hospital in Boston have detected early COPD risk factors in the Hispanic population. As a rule, the condition is found in patients that are over sixty years old, and managing it at that point is challenging. Having explored the results of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), Brigham’s team concluded that previous smoking history, chronic sinusitis, and asthma are the key risk factors of early COPD. To reduce the rising-risks impact, the team recommends raising awareness measures and culture-sensitive bilingual patient education to reach out to the targeted patient populations.
To crown it all
Digital transformation is a complex and costly process that requires efforts from all involved, from patients to clinicians and other hospital staff. However, the benefits it may bring to hospitals undoubtedly justify the means.
In spite of all the hindrances, digital transformation in healthcare is underway and shows no signs of stalling. Luckily, health system leaders now fully understand the complexity of the process and the importance of incremental growth, not just one-time technological solutions. To overcome the challenges of the transformation journey, experts recommend ensuring enterprise-wide participation and consistent patient and employee training. The latter factors foster the technology adoption by both clinicians and patients and their engagement with it.
What is more, having successfully digitalized their facility, medical providers can mitigate such unnecessary cost factors as the failure of care delivery and coordination, overtreatment or low-value care, and administrative complexity.